It’s easy for us as clinicians to feel like we’re falling behind.
That constant feeling like we’re not keeping up.
And no wonder we feel that way.
Just looking at the amount of new information that is created on a daily basis is staggering.
According to a Forbes article, there are 2.5 quintillion bytes of data created each day. (I don’t know about you, but the number seems unfathomable). And there are 40,000 Google searches done every second.
There’s increasing competition within the movement rehab space as well. And our patients are becoming increasingly sophisticated.
The pressure to stay up-to-date continues to rise.
And it can all feel a little exhausting.
It can leave us with a pit in our stomach that we aren’t keeping up.
Social media can help us, but it has a dark side.
The amount of self-help content on Youtube, IG, Tiktok, etc provides both the clinician and the patient with an abundance of exercise ideas, quick fixes, etc. It’s easy to fall into the trap of seeking out social media for more exercises, more assessment techniques, and more treatment options is the solution.
But if we’re not careful, we can find that scrolling through these posts can leave us (myself included!) feeling discouraged and uncertain about ourselves and our skills. A fresh exercise idea can help spur creative thinking, but if we’re not careful we can become consumers of the content resulting in no change in practice.
Part of the problem is how we view ourselves and the value we provide to patients. We can fall into the trap of believing that we need to amass more information.
We believe that our value comes from being a Data Aggregator.
I will show you in this blog post how we can reframe the value we provide to patients that will help you move into a place of greater flow in your practice.
As I’ve reflected on my use of social media and my increased time creating short-form videos, I have observed my internal experience. I noticed a shift in myself with scrolling through various movement-related content.
I felt a sense of inadequacy.
I was left questioning my understanding and knowledge. And I could see how quickly it could begin to impact my sense of self.
Protecting and nurturing our sense of self is crucial.
It’s from a place of safety, stability and support that we can have the fortitude to be curious, collaborative and creative in our clinical practice.
The risk with being consumers of information – especially addictive social media feeds – is that we can become purveyors of information, but not action-takers of that information.
We don’t move past surface-level consumption.
Here’s a graphic that highlights what I’ve found happens with social media and our sense of self as clinicians:
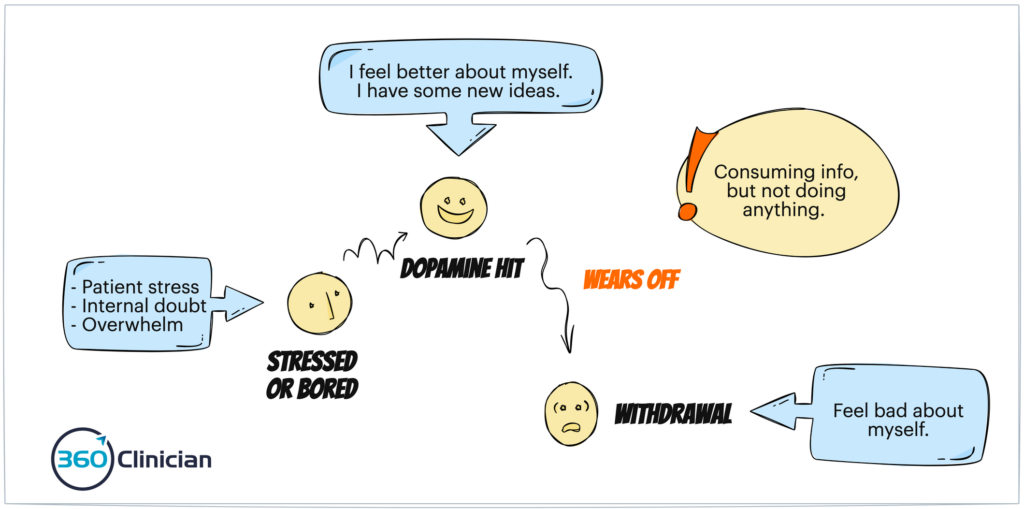
Because of the variable reward mechanisms inherent within social media, this cycle can become quite addictive. And the research is beginning to show the physiological changes to the brain related to social media usage.
While clinical tips and tricks can be helpful, it can be hard to move up the knowledge pyramid in our practice. We can stay stuck in the data and information levels and not move further up into the knowledge and wisdom stages.
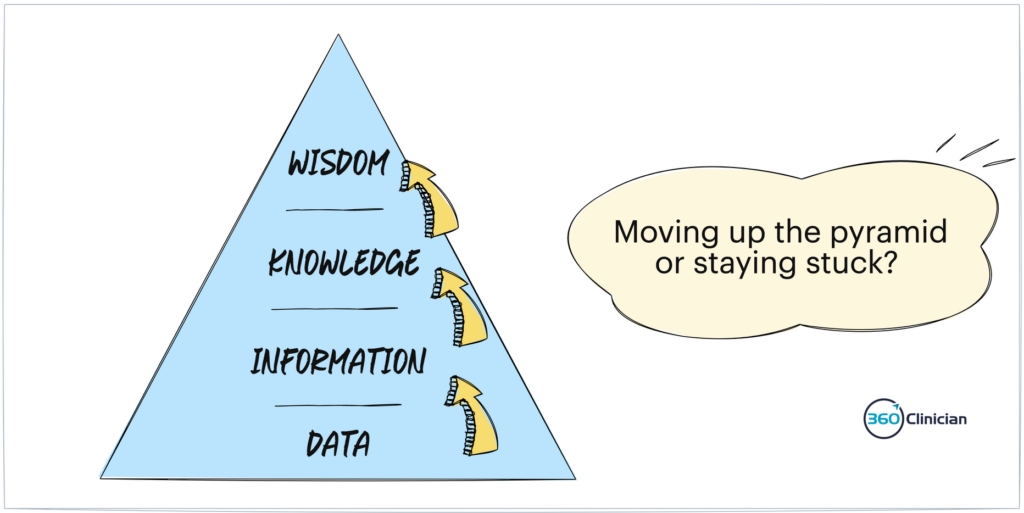
Here’s a sign of being a Data Aggregator.
One of the signs of being a Data Aggregator is that we can find ourselves lost in our clinical assessments.
We do more and more tests and collect more objective data without gaining further clarity. Being unable to make the connections between our subjective and objective data points can leave us feeling more confused than ever.
I remember having a patient transfer to see me for persistent shoulder pain as a result of a car accident.
Her function was quite limited and found that she was still struggling to make progress and return to lifting weights at the gym. I received the chart note and found more than 30 different data points from the last therapist’s objective assessment. But there was no information outlining a clinical picture of what was going on for this patient.
I believe that you open up a new world to yourself when you can re-orient your framing of the value that you provide as a physiotherapist.
We are Sense Makers for our patients.
We need to shift our framing from seeing ourselves as a Data Aggregator to being a Data Integrator.
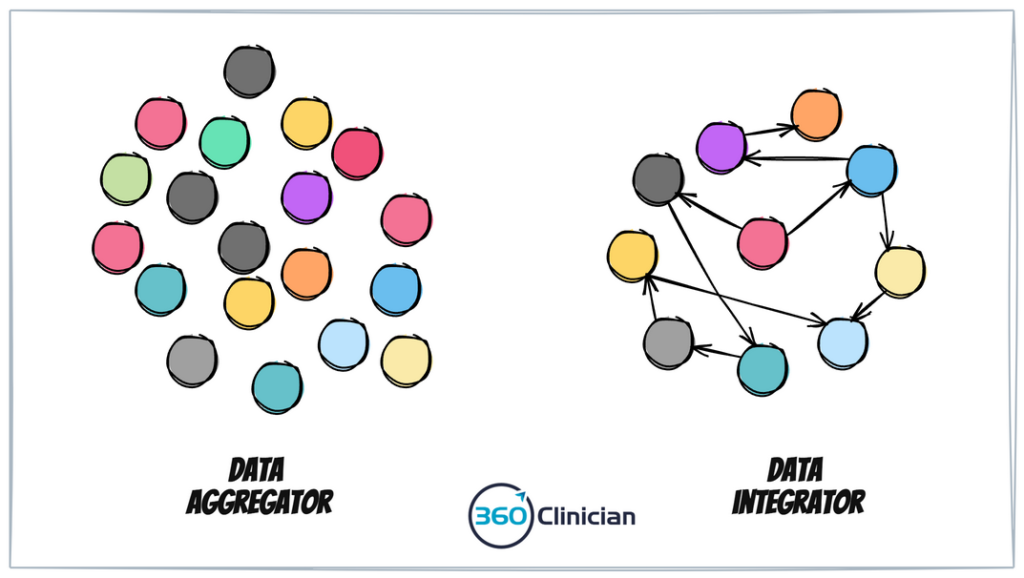
Let’s review what integrator means – it comes from the word integrate – which means to bring the parts together, or to look at the whole.
This is the value we provide to our patients.
As physiotherapists, we are “sense makers” for our patients.
We help to connect the dots for our patients and help to bring a complete picture of movement problems and physical dysfunction.
When we see ourselves as data integrators, it also challenges us to bring a holistic focus to our assessment and treatments.
We help our patients connect the dots and provide insight and understanding into addressing their specific pain or injury and we also help them understand the ‘why’.
We help patients see their bodies in new ways.
There is NO amount of exercise instruction on IG or Tiktok that patients can do that will come near the value that YOU can provide.
Practical Ways to Be a Data Integrator
I want to provide a few concrete suggestions to help you move deeper into your role as a Data Integrator.
First off, if you haven’t read my recent post about the importance of attention and clinical performance then I’d encourage you to do that as there are some important points to improve one’s attention to improve performance.
As I mentioned before it’s important to protect and nurture your inner self. Creating a sense of stability, safety and support will allow you to move into a deeper place of creativity and curiosity. With that in mind, I would recommend being intentional about social media usage.
If you’re looking for fresh ideas and inspiration, be intentional with this effort. And if you find something, capture that insight somehow and look for a way to apply it as soon as possible within your clinical practice. If you’re feeling lost in the endless scroll, or anxious about all the information and opinions out there, then take a break.
2 Antidotes to Improve Sense-Making & Reduce Overwhelm
First off, it can be helpful when going through an assessment to refine the clinical picture you’re beginning to see, by organizing the data points you’re gathering from your subjective and objective examination. As outlined in the article Clinical Reasoning in Manual Therapy combining hypothesis-driven decision-making with an improved organization of knowledge can create superior diagnostic outcomes.
As an example, I’ve found that organizing my physical assessment data points into tissue-based categories is helpful. As I work through my evaluation, I look to see which category appears to have the strongest signal. Is this a joint problem? A muscle problem? A neural issue? As I work through my assessment, I’ll begin leaning towards one of those drivers of dysfunction and then look for both affirming and disaffirming data to refine my diagnostic hypothesis.
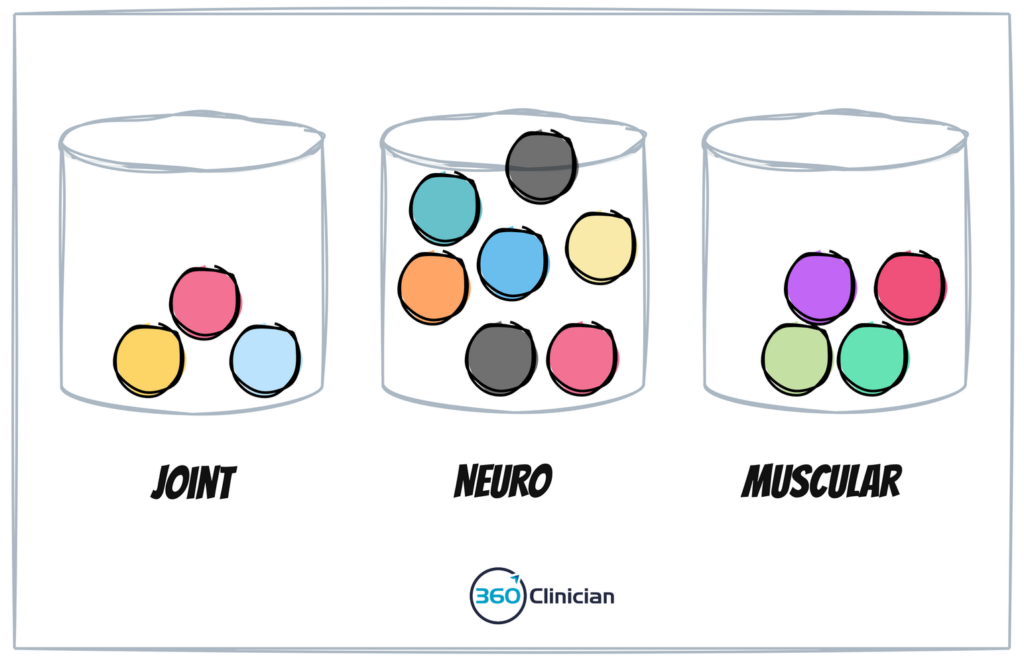
While this process can be done on the fly, it can be useful to work through a clinical reasoning grid to consciously organize your thoughts and prioritize your assessment findings. Once you’ve gone through this process, you can begin to look at the whole picture and start to develop a working hypothesis.
Here is how you can go deeper…
To further your ability to integrate your assessment data, you can begin to map out the possible ‘why’ for your key assessment findings.
For example, let’s say you have a shoulder patient who presents with mild external rotation weakness and tenderness of the supraspinatus. They also present with a mild painful arc. As discussed in my post about adopting a hypothesis-based approach, I could say that I believe the patient is presenting with mild rotator cuff pathology with possible supraspinatus tendinopathy.
From this point, you can then begin to ask yourself what is contributing to your key objective findings. I find that getting pen and paper can be helpful tools to support working through this.
You would outline your diagnostic impression along with your most salient objective findings. For each of these findings, you would then look to better understand potential drivers for that objective finding.
Here is an example of working through one objective data point for our shoulder case:
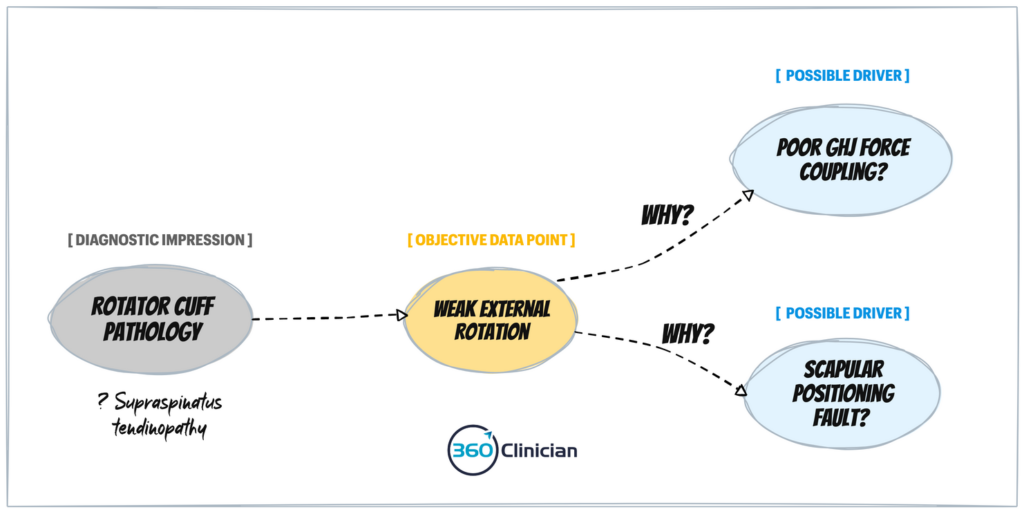
Once you have this mapped out, you can begin to work through your treatment planning approach and identify which drivers are most important to create change with your objective findings.
Keep in mind that this is an iterative process that may change during your assessment and treatment planning as new data points become available. The goal is not to be dogmatic with your clinical reasoning, but rather to be flexible and open to new information.
In Summary
Remember, that your value comes from deepening your skill and experience in being a Data Integrator. Once you reframe how you view yourself and the value you bring your patients, you will be free from the weight of feeling overwhelmed by the constant barrage of messaging that says you don’t know enough and that you’re not enough.
From this place of security and support, you will be able to move into a deeper place of creativity and curiosity. This is where your best ideas will come from. When you are free to explore and be curious, your patients will benefit the most.
To Greater Flow,
Andrew
If you enjoyed this article and want to stay up-to-date on my newest content, sign up for the Clinical Flow Newsletter! There you will have access to special offers, exclusive content, and be part of a growing community of clinicians with the purpose of improving yourself and your clinical practice.