Discomfort.
Self-doubt.
Overwhelm.
These emotions can be present with us every single day… often to varying degrees with every patient. Unfortunately, these emotions can hound us as physiotherapists.
We are constantly dealing with discomfort, uncertainty and even overwhelm in our clinical practice.
And part of the problem is that no condition presents the same.

Take a patient with a partial rotator cuff tear.
What can seem routine at first glance becomes more challenging when you add poor patient kinesthetic awareness, poor patient motivation and challenging work demands. These uncertainties can shift our state from one of flow to one of dis-ease and distress.
In today’s post, I’m going to identify the unsuccessful ways we use to deal with these emotions. I’ll outline the three common Distress Accelerators that make things worse. And finally, I’ll show you three strategies to reframe how you interact with uncertainty and discomfort and tame the beast of overwhelm.
So let’s get started…
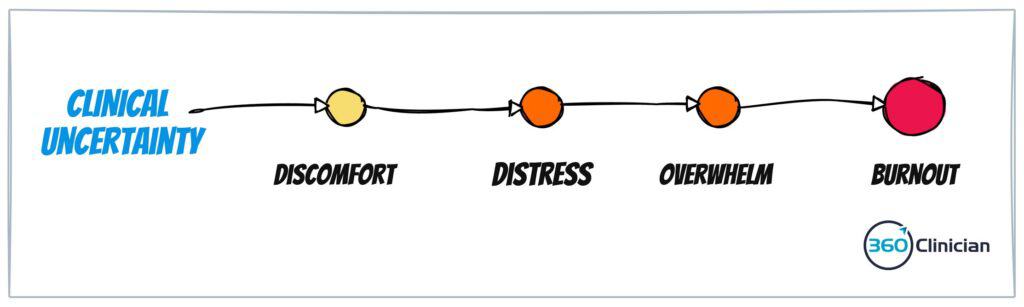
If we don’t manage the emotions of discomfort and distress well, we can experience overwhelm. And overwhelm can lead us to burnout.
So what do we do when these negative emotions creep in?
A popular misconception is that the solution to these emotions is acquiring more knowledge. We believe that our uncertainty, self-doubt and overwhelm is because we lack the ‘right information’. We seek out courses as the solution. While new information can be important, it often times is not the answer.
Second, we try to boost our confidence levels. We believe that the antidote to these emotions is to improve our self-talk and bolster our confidence. But we quickly realize that mustering confidence is not a long-term winning solution.
And finally, we try to eradicate uncertainty. I know for myself, there was a drive early on to try to overcome uncertainty and doubt. It’s easy to start comparing ourselves to other therapists as we see them exuding confidence in their assessments and treatments. Things can appear black and white. And we erroneously believe that a “good” therapist should have no hesitation or self-doubt. This belief can be further reinforced by the pressures of feeling like we need to have all the answers for our patients.
The Shift from Discomfort to Overwhelm
It is normal to feel uncomfortable when confronted with clinical uncertainty. Discomfort in our clinical environments is inevitable. However, when that discomfort starts to shake our confidence and prevent us from handling situations correctly, we experience negative emotions like anxiety or overwhelming distress. The buildup of stress can lead to emotional exhaustion, which is a key symptom of burnout.
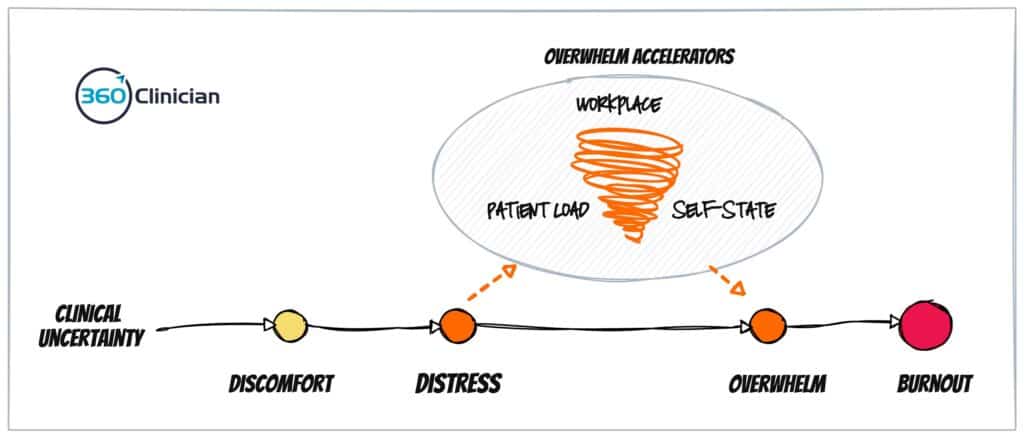
So how does one move to a place of distress and overwhelm? I believe there are three Overwhelm Accelerators that can impact the amount of uncertainty we can handle:
First off our work environment. Unfortunately, when we are multi-tasking, such as seeing multiple patients at once, we can end up being unable to attend to the uncertainty we experience. As discussed in my last blog post, we end up being in a reactive, sympathetic state more often than we would like. This can lead to limited attention capacity and decreased problem-solving capacity.
Next up, our patient caseload may be too challenging or complex and may not be well suited to your skills or personality. While a certain amount of uncertainty is normal, experiencing constant, unrelenting uncertainty will make it more difficult to develop the resilience required to withstand the challenges of an ongoing clinical practice.
Finally, our self-state (e.g. our sense of being) is another key aspect that impacts how we handle uncertainty in our clinical work. When we have a strong, centered self-state we are able to withstand the challenges, both internal and external, that come our way. When our self-state is less robust, we can quickly become defensive and react to seemingly small things.
So how do we stay in the sweet spot, where we are neither too comfortable nor too overwhelmed?
3 Ways to Stay in the Sweet Spot
First and foremost, it is important to understand that these emotions are normal and part of clinical work.
You are not alone in feeling this way.
There are so many pressures on us, and those we place on ourselves, that we can often feel like we’re not measuring up. And this pressure can make it even more challenging to navigate the internal world of discomfort and distress that can begin to ooze into every part of our clinical life.
So let’s dive in!
#1 – Lean into the discomfort
Challenging our beliefs about discomfort and uncertainty can unlock a new understanding that will improve our clinical experience. If we accept that uncertainty and discomfort are normal and expected in clinical practice, we can begin to shift our relationship to these experiences and emotions.
Rather than pushing away discomfort and uncertainty, see it as an invitation. Authors Ilgen et al, in their article Warning bells: How Clinicians Leverage Their Discomfort to Manage Moments of Uncertainty highlight the importance of tuning into the dance between comfort and discomfort. The clinicians in their study were:
Able to ‘manage’ experiences of uncertainty by monitoring the evolving balance between discomfort and comfort during these moments, continually revisiting and revising their sense of whether their management approaches were working.
So what does this look like practically?
I found personally, that the only way to welcome discomfort into my experience, is to see it as a friend and not a foe. It is about moving out of a place of rigid mental models and moving to a place of agile and open thinking.
Simple mantras here can make a big difference. Repeated phrases, or affirmations, help keep us focused on the state we want to maintain. For example, reminding yourself that “discomfort is ok” can be a good place. Often we can find our perfectionistic tendencies keeping us back and the mantra “It’s ok not to have all the answers’ can be a powerful antidote.
This is also where understanding our self-state is crucial.
I find that internally acknowledging the discomfort I am feeling is an important first step into acknowledging and embracing discomfort. Often there is a pre-cognitive experience that we can feel – a tightening in our chest, a shift in our breathing, or a visceral discomfort. Acknowledging the bodily sensations can be a helpful gateway to exploring the discomfort cognitively. Finally, take time to process the discomfort outside of the pressures of a patient in front of you. I think one of the biggest mistakes I’ve made is pushing these emotions away and thinking that being away from the clinic or a night’s sleep will solve the problem.
Accepting discomfort & uncertainty is part of the journey. It’s not possible to be certain about everything all the time. And that’s OK! When we can sit with the discomfort and not try to push it away, we can start to get more comfortable with it.
#2 – Focus on hypothesis-driven decision making
One of the biggest changes I’ve found in my own clinical practice has been adopting a hypothesis-driven decision-making process, otherwise known as the hypothetico-deductive (HD) method. We are constantly dealing with imperfect and incomplete information. By approaching our assessment findings and diagnostic impression as a hypothesis to be tested and confirmed we can shift away from one right or wrong answer. It also takes some of the pressure off as you adapt to new information that becomes available during a course of treatment. This approach acknowledges uncertainty and gives you the space to respond to discomfort. This then allows you to adjust and refine your diagnostic hypothesis based on confirming or disconfirming information.
So what does this look like practically?
Shift the language you use with your patients: I incorporate hypothesis-oriented language with my patients. This includes using words like “my impression of what I’m seeing is X based on XX. I want to provide treatment X and then re-evaluate to see if there any changes.”
For myself, I find how I talk to myself about my assessment findings is crucial. I use self-talk that includes “assessment hypothesis”, “testing my hypothesis,” etc.
I embrace doubt in my assessment findings. I want to challenge my thinking and I want to avoid holding on too tightly to a particular diagnosis.
In my group coaching program for therapists, I help therapists create a decision-making map to help take the stress out of how to assess and treat patients.
If you feel especially distressed during a patient assessment or feel stumped, ask yourself this question: “What is ONE thing that I could do to begin moving the needle for this patient?” This can help to focus your attention and decrease the data overwhelm that can paralyze us.
#3 – Address one or more of the Overwhelm Accelerators
Another important antidote to reducing distress and overwhelm is looking at the 3 Overwhelm Accelerators that I introduced earlier: your workplace environment, your patient caseload and your self-state.
Let’s dive briefly into changes you could make across each of these accelerators:
Workplace: Sometimes there are changes you can make and sometimes there are not. Knowing the difference can be a challenge. It’s important to focus on things you can change to see if you reduce your distress and overwhelm.
- See fewer patients per hour – increase your assessment and treatment session length
- Avoid double booking patients
- Add a break after three patients so you can have a buffer before your next group of patients
- Give yourself a physical break in your clinical day for a chance to eat, drink and have a few moments of mental and physical pause
Patient Load: The types of patients you’re seeing can alter the amount of uncertainty you’re experiencing. Ask a more seasoned therapist to see your patient while you’re observing their approach – ensure there is an opportunity to debrief and reflect afterwards to deepen your learning.
If you’re seeing a certain type of patient population that you find particularly stressful, see if you can have the clinic reception reduce the number of those types of patients. If you have a particular type of patient that you find energizing with less uncertainty, then let other therapists in your work setting know this and identify ways to market your specific skill in treating patients with that clinical presentation.
Self-State: Your self-state is an important modulator to managing uncertainty and discomfort. Learning the contours of your inner self is necessary, but it is challenging work. And it’s easy to brush aside.
Here are a few ways to explore the inner self and improve how to navigate clinical uncertainty:
- Complete a short, end-of-clinic day meditation
- Carve out 10-15 minutes to journal about a particular patient situation
- Identify strategies to increase your physical, emotional and spiritual energy stores.
The key is to focus on the things you can change: your workplace environment, your patient caseload and your self-state. Implementing small changes across each of these areas can help reduce your clinical distress and overwhelm.
The Wrap Up
Dealing with uncertainty, discomfort and overwhelm is tough and draining. But ignoring these emotions, especially if they’re chronically elevated leaves us at risk of burnout.
Leaning into discomfort and taking a hypothesis-driven decision-making approach helps give us the much-needed space to manage the dance between discomfort and comfort. And finally, I hope that exploring the impact of the Overwhelm Accelerators on your emotional state can give you some practical areas of change so you can increase your clinical flow and enjoyment.
To Better Flow,
Andrew
If you enjoyed this article and want to stay up-to-date on my newest content, sign up for the Clinical Flow Newsletter! There you will have access to special offers, exclusive content, and be part of a growing community of clinicians with the purpose of improving yourself and your clinical practice.