Myotome testing is often seen as a necessary, but not always insightful element, of a shoulder assessment.
It’s easy to fall into the trap of seeing myotome testing as optional for the shoulder patient — especially if there doesn’t seem to be any suspected radicular or peripheral neuropathic indications from the patient history.
Do you find yourself checking any of these boxes?
- Feeling pressured to leave out myotome testing because of limited time.
- Avoiding myotome testing because of pain potentially confounding results.
- Not sure of the value of myotome testing beyond typical C5 involvement.
Then you’ll want to keep reading to learn how you can use myotome testing to gain fresh insights and gain more confidence treating painful shoulders.
To help improve my ability to connect the dots in my clinical assessments, I’ve come to more deeply integrate myotome testing with every shoulder patient. For me, myotome testing has moved beyond identifying frank neurological issues towards understanding the role that neurological function can have on muscles and tissues impacting shoulder movement, strength and function.
In this blog post, I’ll be sharing why skipping out on myotome testing can be a big mistake for shoulder patients and why we need to look beyond the typical myotomes related to the shoulder to improve our clinical assessment outcomes.
The 4 Mistakes That We Make with Myotome Testing & Shoulder Pain
Mistake #1: Assuming neurological involvement isn’t there
I think it’s easy to dismiss neurological involvement with shoulder patients. They may have weak and painful shoulder external rotation and abduction which may confound our ability to identify possible neurological influences. But other nerve root levels can be involved that can impact shoulder movement.
Since being trained in GunnIMS over ten years ago, I’ve gained a deeper appreciation of the nervous system’s role in affecting muscle tone. Even mild spinal root irritation can influence muscle tone of those the muscles supplied by the affected nerve root distribution. Increased muscle tone can result in decreased muscle length which can influence shoulder biomechanics.
Mistake #2: Going too quickly through myotome testing
I have found that it’s easy to go too quickly through myotome testing. When time is limited, we try to be efficient. However, in that quest for efficiency, it’s easy to give a cursory look at a narrow set of myotomes. Incorporating a greater number of upper extremity myotome levels will help give you a broader perspective of contributing factors affecting the shoulder.
Mistake #3: Not adapting to more sensitive testing positions
As mentioned in Mistake #2, we can go through testing too quickly. We were taught in school to go through myotome testing in sitting. An efficient body positioning standpoint doesn’t necessarily allow us to pick up on subtle fatiguable weakness. Optimizing our body mechanics becomes even more important when looking to identify fatiguable weakness with patients bigger and stronger than ourselves.
Mistake #4: Seeing it as a basic skill and not refining application within assessments
Since myotome testing is something that is covered early in orthopaedic training, it’s easy to see it as a basic skill. I believe that there is real value in revisiting these ‘basic’ skills to understand how to refine the approach used, as well as its role in helping to connect the dots in our shoulder assessments.
Why are Myotomes Such a Powerful Tool for Shoulder Assessments
There are three reasons why elevating the use of myotome testing can improve your shoulder assessments.
First off, cervical myotome testing helps you identify the contribution of neurological impacts on muscles affecting the shoulder girdle. When you’re identifying movement restrictions with shoulder testing, you’ll be able to better sense if the movement restrictions are a result of cervically-mediated muscle tone changes.
Second, myotome testing is an excellent way to incorporate testing-retesting into your assessments. Patients can appreciate the visible fatiguable weakness of muscle testing during your assessment. As well, this testing is typically done on non-irritable muscles outside the shoulder girdle.
Finally, addressing the cause of the myotomal disturbance can be starting point with treatment and can give you a quick win with your patients. There are a variety of ways to influence neurological function. Patients can see an improvement with these measures which helps build trust and confidence in your skills.
How do Myotomes Impact Your Shoulder Assessment & Treatment
When looking at the shoulder complex, the rotator cuff muscles are innervated by C4, C5, C6. The deltoid is innervated by C4, C5, C6, C7 and the latissimus dorsi is innervated by C6, C7, C8 (bold highlights indicating primary innervating segments) (Gunn).
Neuropathy and radiculopathy can result in nerve disturbances including super sensitive nerves and innervated structures which Chann Gunn outlines in his book The Gunn Approach to the Treatment of Chronic Pain. His radiculopathy model is based on Cannon & Rosenblueth’s Law of Denervation which states that the function of innervated structures is based on the free flow of nerve impulses (Dommerholt et al, 2006). It is hypothesized that these disturbances can result in increased muscle tone and altered muscle length within the affected distribution.
A Clinical Example
Let’s look at someone with some contribution of poor cervical posture (e.g. head forward posture). With this posture, there can be increased irritation at the lower cervical joints, specifically C7-T1.
With myotome testing you would pick up on some fatiguable weakness potentially at C7, C8 and perhaps even T1.
When looking at the muscles innervated at those levels, we must take note of the latissimus dorsi.
The latissimus dorsi is a muscle that is notoriously hypertonic and shortened, especially in individuals with poor cervical and thoracic alignment. Given the nerve root supply of the lats muscle (C6, C7, C8), the influence of the cervical spine on this muscle can create a feedback loop that perpetuates shoulder, scapular and cervical dysfunction.
Clinically, I found that the lats, when hypertonic due to neural irritation, corresponds consistently with positive myotome testing at the C7 level.
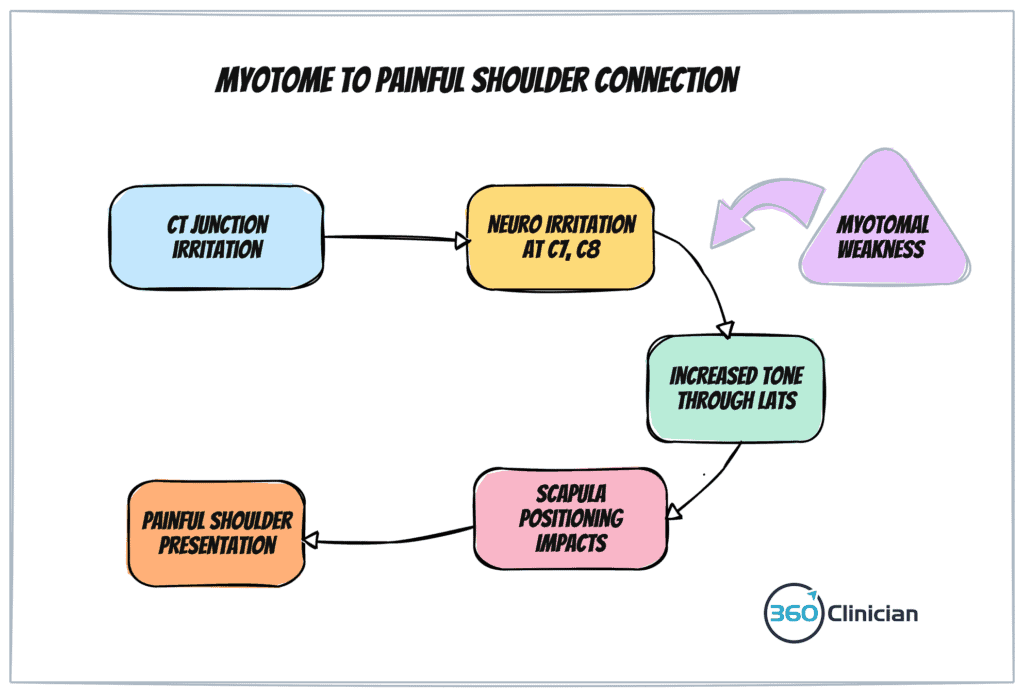
The lats can contribute to disruption of the scapulohumeral rhythm as well as increase shoulder girdle depression. It can also alter scapular elevation resulting in increased resistance when performing overhead movements of the shoulder (Sahrmann, 2002).