Do you find it challenging to assess and treat patients with ‘insidious onset’ pain?
Do you find yourself frustrated with understanding how things are connected during your assessments?
When patients complain of ‘tightness’, ‘stiffness’ and ‘pains and aches’ without a specific mechanism of injury it can be challenging. In part because the complaints can often feel vague.
To become a detective in understanding the clinical presentation, it’s important to use a systems thinking approach.
Systems Thinking & Feedback Loops
A helpful lens to look through when it comes to clinical reasoning in these situations is to think with a systems perspective. A system is a set of things interconnected in a way where they create their own pattern of behaviour over time. A system has inputs which interact with each other and create a set of consistent outputs.
A systems perspective recognizes the inherent inter-connectedness of the various parts of the system. Systems thinking helps us move beyond the pain site to understand drivers and contributors to one’s pain experience.
One of the central aspects of systems theory is that of feedback loops.
One of the key concepts of systems thinking is feedback loops, which are circular processes that amplify or dampen the effects of an action or a change. Feedback loops can be reinforcing or balancing, depending on whether they increase or decrease the gap between a desired and an actual state.
Often, multiple feedback loops interact with each other to perpetuate poor movement patterns, joint stiffness, muscle weakness, neurological irritation, etc.
A Clinical Example
Let’s say that we have a patient with poor hip mobility.
He has been doing intense cardio using his peloton bike and complains of lateral right low back pain.
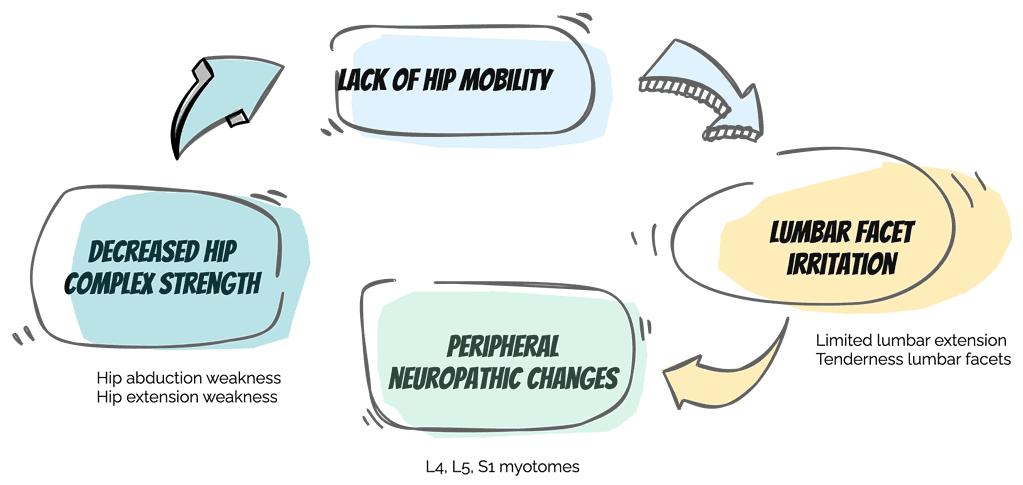
On examination, he has limited hip mobility along with decreased hip strength. His lack of hip mobility is influencing his lumbar spine. How do we know this? In part, by the neurological exam that shows myotomal weakness on the right, specifically L4, L5, and S1 myotomes.
So here we have a system at play:
The lack of mobility in the hip contributes to peripheral neurological changes that impact hip complex strength. This decreased strength in turn impacts joint stability and support because of the decreased muscle support.
One feeds the other.
Here’s a visual to highlight the system at play:
Creating a Pattern Interrupt
The goal now is to understand how to change this feedback loop.
How do we create a pattern interrupt that disrupts this interaction effect between the hip and the low back?
A simple movement pattern I used with this patient was rocking on hands and knees with the goal of improving hip movement without flexing through the lumbar spine. It’s simple to do, it’s non-irritating to the hip or the low back and can be done easily by the patient.
Just like psychological pattern interrupts can help us get out of ruts with our thinking and behaviour, the pattern interrupt within the treatment context is one that allows us to get out of the revolving loop that can limit improvement and function.
In this case, I wanted to assess the ability of a simple hip hinge movement pattern to alter the neurological function of the lumbar spine. It was simple, non-irritating to the patient. I retested the myotomes following this simple test, and then I retested hip strength. Both had improved, and I knew I had a valuable intervention to begin altering the present feedback loop.
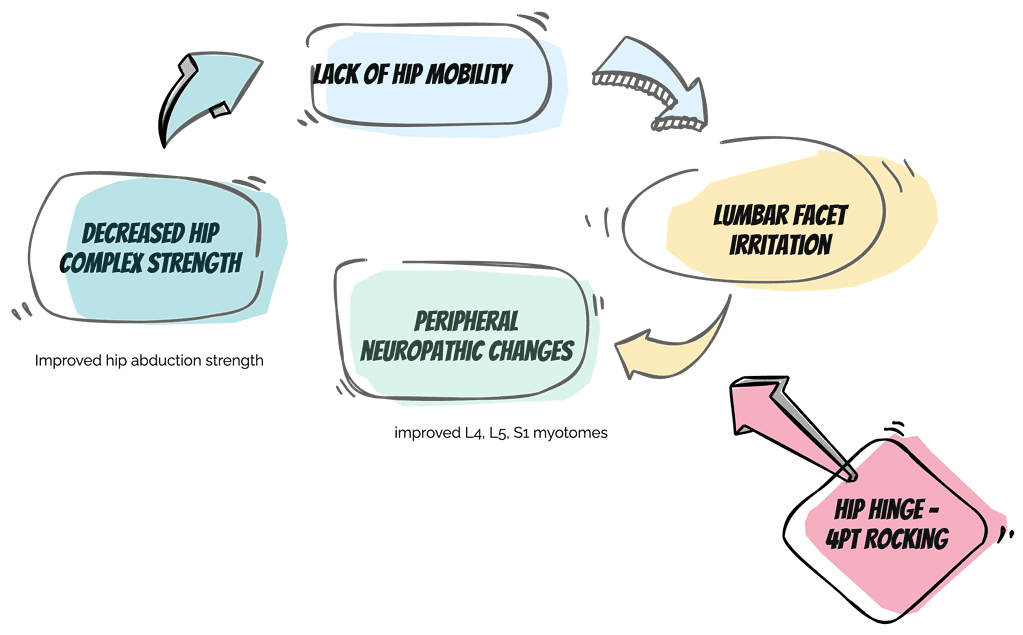
From this simple intervention, we can begin to increase our confidence in unravelling complex movement system issues.
What’s your experience with dealing with insidious onset pain? What did you do about it and did you find it worked?
I’d love to hear from you so feel free to drop me an email🙂

