In my last blog post, I introduced the concept of a clinical reasoning framework and how it can help you reduce decision-making overwhelm and fatigue. I outlined why it’s important to develop your own clinical reasoning framework and the benefit of owning your framework.
Today, I want to walk through the three key building blocks of one’s clinical reasoning framework.
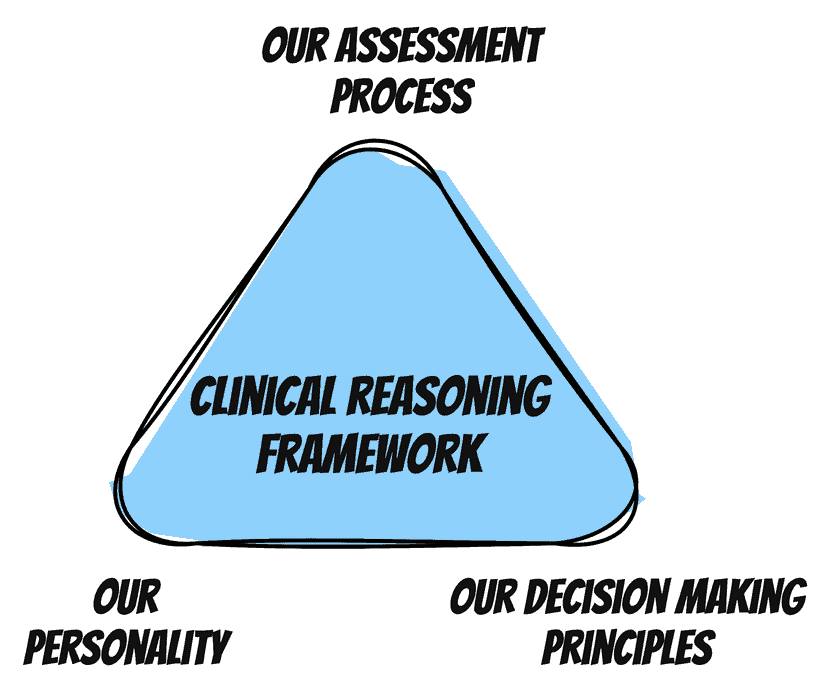
Our Assessment Process
First off, let’s talk about the process we apply to our assessment and treatment planning.
Our assessment process is one that at a high level is already quite defined. We go through a history taking, followed by a physical exam, then an explanation of our findings and treatment plan. This is then followed by initial treatment as time allows. Within this overall structure, we can explore how to define our process in more detail.
When doing an assessment, we evaluate the body area in question, but also how we integrate our neurological exam and functional screening. As mentioned in a previous blog post, there are different ways to zoom in and zoom out during a physical exam to help you get a better handle on the interconnectedness of the body and the patient’s pain and dysfunction.
We also develop a structure to our treatment plan. It is a valuable exercise to ask yourself these questions to better understand the treatment planning process:
- How do you choose which exercises to do?
- What determines your next step from a treatment planning standpoint?
- Do you have a process for when to integrate hands-on and when to transition away from a hands-on approach?
Our Decision-Making Principles
Principles help make our decision-making easier because we can rely on principles even when we see a condition or presentation that is different than something we’ve seen before.
We learn and refine the principles we rely on from many sources: from our entry-level education, ] from additional courses we take and from our lived experience. Often we’re not conscious of the principles we employ. Becoming more conscious of the principles we’re engaging with can help us to operate with greater clarity and more calm.
It can be helpful to ask yourself these questions to better understand the principles you’re using:
- What principle did I use when I was dealing with a condition that I wasn’t as comfortable with?
- What rule-of-thumb did I use when progressing a patient’s treatment plan?
- What principles did I employ when completing a differential diagnosis during a previous assessment?
Our Personality
Our personality is something that we don’t often consider in a clinical reasoning framework, but it’s something important to consider. There are certain ways of approaching clinical reasoning that may not jive with how you think and how you process.
I think it’s important that the framework that you build plays to your strengths and your natural cognitive processing tendencies. A clinical reasoning approach that is highly technical and requires recall of minutia may work well for one clinician, but may not work well for someone else. This can apply similarly to an approach that requires very subtle and skilled palpation skills.
Adopting another’s clinical reasoning framework that incorporates a style of treatment that isn’t congruent with who you are or your personality style will result in regular frustration and overwhelm. It’s not to say that you couldn’t improve certain skills or stretch your comfort level to some degree with practice, but recognizing our own limitations frees us to embrace a style of practice that is congruent and enjoyable for us.
A few questions to help you better understand this area include:
- What kinds of treatment approaches frustrate me?
- Do I gravitate to a particular treatment approach? Is there a pattern that I can identify?
- What styles of treatment am I drawn to in my colleagues? What do I find attractive about them?
What should I do now?
When you’re looking at the overwhelm, discomfort or cognitive fatigue you experience with clinical work, ask yourself which area could be contributing to these emotions.
- Is it your assessment process?
- Is your assessment and treatment approach jiving with your personality?
- Are you feeling fuzzy about the decision-making principles you’re using?
Let me know what you come up with in the comments below, I’d love to know!