You’re looking at the assessment data you’ve scribbled on your sheet of paper or in your EMR.
Feelings of anxiety and overwhelm start to bubble to the surface.
You’ve gone through all your standard subjective and objective assessment steps. You’re seeing some obvious things, but you’re not really sure how it all fits together… or if it does at all?!
Your patient is looking to you for certainty and confidence, but you’re feeling anything but that at the moment.
If you’ve felt this recently, then know you’re not alone! And it’s not just a new grad experience. We all have these experiences.
Discomfort is a normal experience when we’re doing clinical work as I’ve written about before.
It’s not a pleasant feeling and naturally we look for ways to experience more certainty.
Here’s a common answer, but does it work?
Gurus claim to have the answers to unlock better clinical outcomes and more certainty. And there are systems of treatment such as McKenzie, Maitland, Integrated Systems Model, etc. that aim to provide you with a complete system of assessment and treatment.
We naturally turn to the gurus and treatment systems because they promise to ease our pain and uncertainty.
Unfortunately, we can find ourselves struggling after taking their training because what sounded so simple in theory is a different story because of our clinical environment, our patient population, and for our personality.
I’ve had it happen many times in the past where I’ve taken a course and then reality hits. What was promised to be an oh-so-effective technique, exercise or approach didn’t pan out.
You were left wondering where things went wrong.
More often than not we can feel that it’s our fault. That somehow we just weren’t good enough.
We can then end up believing that we didn’t implement things perfectly so we try even harder. Unfortunately, I don’t think it will give us the confidence and certainty we’re looking for.
Why? Because we don’t have the same lived experience, knowledge and thinking pathways of the guru or thought leader who developed the framework.
Why we need a clinical reasoning framework
While we can adopt certain parts of an existing framework, I believe we need our own clinical reasoning framework that honours and fits our unique personality, lived experience, patient caseload, and training.
I believe that our clinical reasoning framework is a living and breathing entity. It’s constantly being refined and added to. To me the real excitement and interest in professional growth is the journey of further developing and refining my own clinical reasoning framework.
A clinical reasoning framework helps you to organize your clinical knowledge base. As Mark Jones and his co-authors share:
Well-structured knowledge is essential to domain competence. Research in cognitive psychology and artificial intelligence, categorization, expertise and education have collectively demonstrated the importance of well-developed knowledge to successful performance.
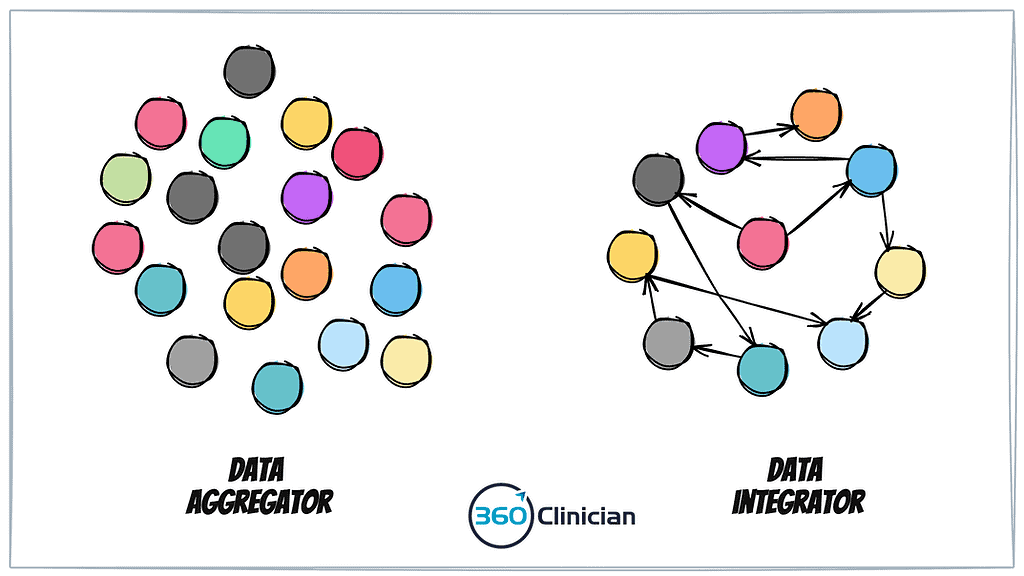
Well-structured knowledge is not simply how much an individual knows but how that knowledge is organized.
Jones et al, (Clinical Reasoning in the Health Professions, 4 ed.)
And that is the crux – gathering more and more knowledge is not helpful to performance unless it is organized in a way that is easily accessible and useful in the clinical moment it is needed. And our ability to access the knowledge we need requires mental scaffolding that is easily navigated and accessed.
3 benefits of owning your clinical reasoning framework
There are a number of benefits of developing one’s own clinical reasoning framework.
First off, it helps to reduce the stress related to dealing with unexpected and complex situations. When we’re dealing with complex situations, we need to know how to approach our assessment and treatment. It can be easy to get blown and tossed by the wind when we don’t know which direction to go. Having a framework to organize and process the clinical presentation in front of us can help us to stay curious and present with the patient.
Rather than having a long list of assessment data points, we can organize our data points into categories and understand relationships between data points to begin creating a clinical story.
We can begin to connect the dots.
Another benefit of having a clinical reasoning framework is that it allows you to better identify areas of strength and weakness within your practice. You can begin to understand where things feel less smooth in your assessment and treatment planning. By recognizing where you find yourself grasping or questioning next steps, you can step back to better understand some further reflection.
And finally, a clinical reasoning framework enables you to actively develop and evolve your clinical reasoning sophistication over time. New information and knowledge can be integrated into your framework and can facilitate more rapid learning and growth.
Rather than having disparate chunks of information that can feel isolated and siloed, a clinical reasoning framework allows you to identify where new learning can fit into your evolving framework.
To better flow,
Andrew