It sucks when you get thrown for a loop with a patient. They can throw off your day and it can feel hard to bounce back from these encounters.
It can be especially unsettling when flare-up symptoms are more dramatic than expected.
I had such a situation happen a few weeks ago, and I wanted to share how I navigated my thoughts and feelings.
I hope you find it helpful!
How it started
It all started on a sunny Saturday morning 🙂
I was getting ready to go to the beach with the family. I did a quick email check before heading out (I have a bad habit of checking email too often). I got an email from a patient who I had seen a few days earlier. He was an older gentleman who informed me he was cancelling his appointment for the following week as his symptoms had gotten much worse after his last treatment session.
I gave the patient a call to find out more about what was going on. He indicated that previously normal movements were now irritable, and his sleep became significantly disrupted after the last session a couple of nights ago.
I felt a pit in my stomach listening to him share this.
What had I done?
My mind raced quickly, reviewing my treatment a couple of days earlier. There was nothing out of the ordinary – everything was movement based and focused on repetitive non-irritable movements.
In those moments, I felt my anxiety increase as I wondered what had triggered this significant increase in symptoms. I offered to see him to help provide some treatment to relieve symptoms, but he declined and indicated that he felt like a guinea pig. Ouch!
Needless to say, I was a little rattled after this experience.
Here’s what I did next
Have you been there before?
Something goes sideways with a patient experience and you’re left reeling a little (or a lot).
Oftentimes we just try to muddle our way through the feelings, or we suppress or numb our feelings. Either way, it throws us off kilter making it hard for us to be present with upcoming patients or with our family and friends.
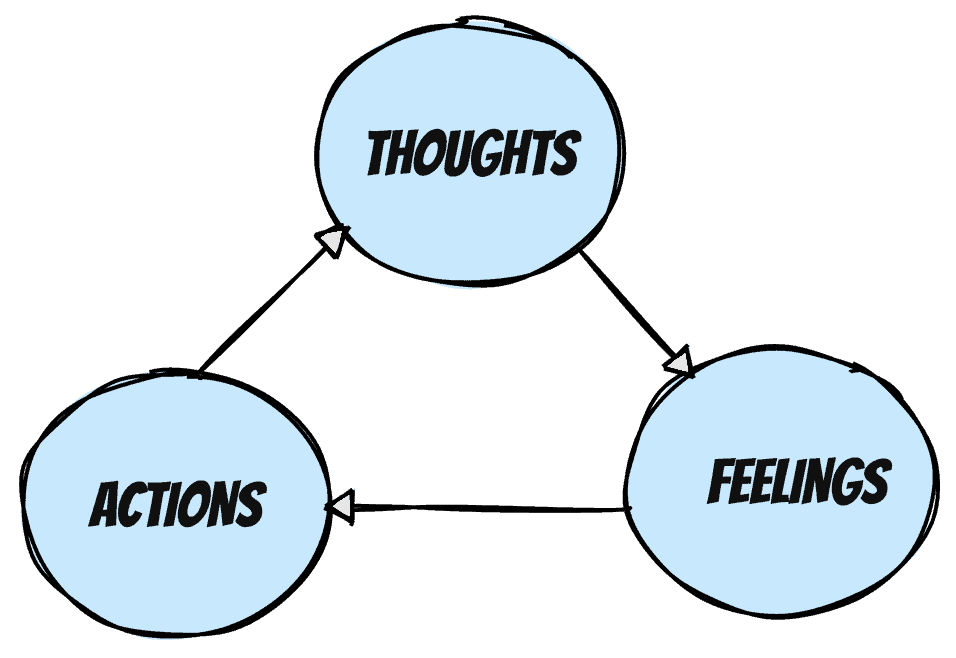
A number of months back I talked about the power of beliefs and the impact they have on our ability to stay clinically agile. The cognitive behavioural model highlights that our thoughts influence our feelings which influences our actions.
The situation felt pretty uncomfortable – I was faced with a choice.
Do I ignore my feelings and wait for time to create enough emotional distance or do I work through my thoughts and feelings and challenge my cognitive distortions – which there were many!
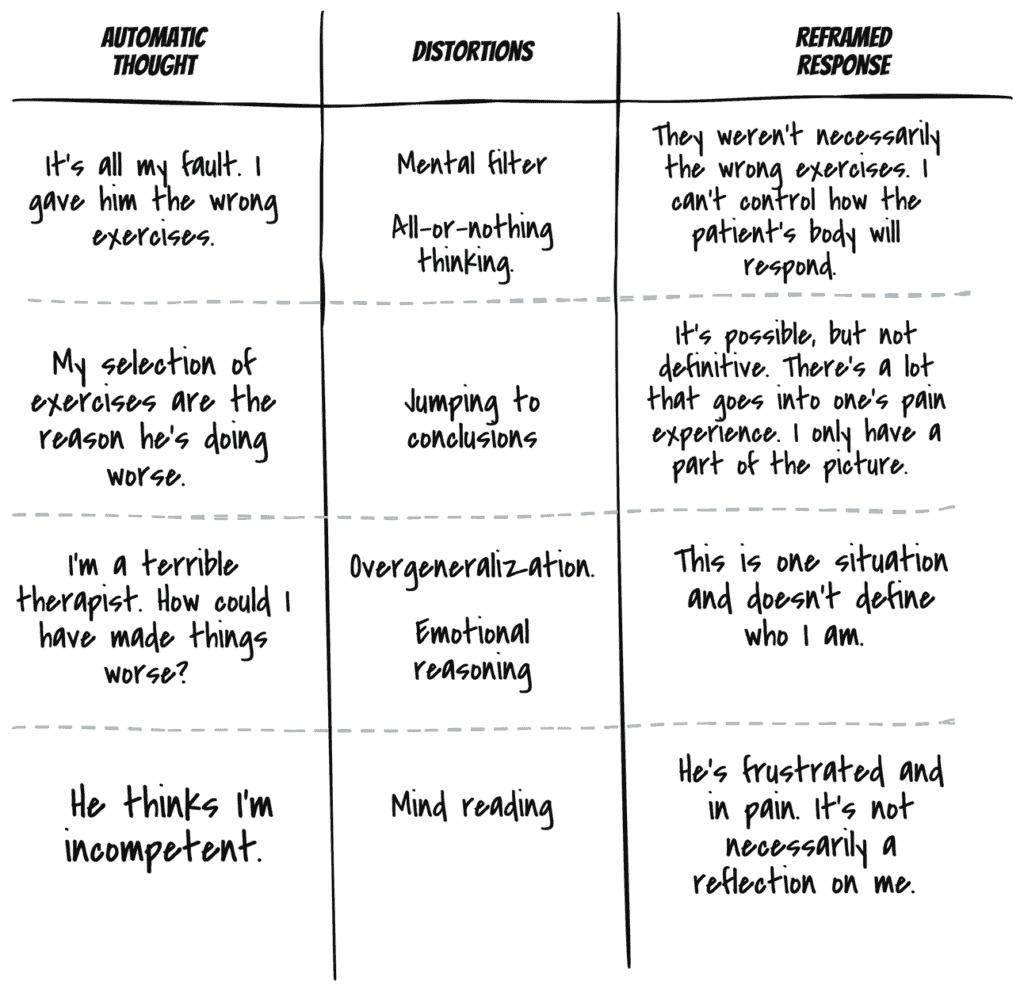
The framework previously discussed looks at identifying your automatic thoughts, the associated cognitive distortions and then reframing the belief more realistically and accurately. Click here to view all 10 Cognitive Distortions or here to read my previous blog post that sheds some light on the topic.
I took out my journal and began the process.
I first wrote down my feelings. In those moments after the phone call, I felt a good amount of anxiety. I was disappointed with myself, I felt embarrassed and I was sad that my patient was suffering.
I then went through the 3 column technique and listed all the thoughts going through my head. Be forewarned, they weren’t particularly rational, but that’s the reality. Writing them down helped me to get these thoughts out of my head onto paper so I can start to look at things more rationally.
Here are four automatic beliefs that were going through my head:
☢️ It’s all my fault. I gave him the wrong exercises.
Distortions: Mental filter. All-or-nothing thinking.
Reframed Response: They weren’t necessarily the wrong exercises. I can’t control how the patient’s body will respond.
☢️ My selection of exercises is the reason he’s doing worse.
Distortions: Jumping to conclusions.
Reframed Response: It’s possible, but not definitive. There’s a lot that goes into one’s pain experience. I only have part of the picture.
☢️ I’m a terrible therapist. How could I have made things worse?
Distortions: Overgeneralization. Emotional reasoning.
Reframed Response: This is one situation and it doesn’t define who I am.
☢️ He thinks I’m incompetent.
Distortions: Mind reading.
Reframed Response: He’s frustrated and in pain. It’s not necessarily a reflection on me.
Here’s a summary of the above in the 3-column technique:
What was the result?
Early in writing things out, things still felt quite intense emotionally. But as I reviewed the associated cognitive distortions and then began reframing those thoughts, the emotional intensity decreased.
It didn’t resolve my emotional experience, but the intensity went way down and I was able to be more present with my family during our beach time.
My inner critic will often get pretty noisy and say that this process will take too long to complete. The reality though is that not going through this process is way more costly in both time and emotional resources.
My journaling process only took about 10-15 minutes which is much less time than I would have spent stewing over the situation and being distracted emotionally from my other interactions.
What could you do?
If you’re interested in exploring this approach to help you navigate challenging clinical situations, I’d encourage you to find a recent situation you’ve encountered that you could walk through. It’s much easier to do this exercise when emotional intensity is less so that you can become comfortable with the mechanics of the process.