I don’t know about you, but I find that it’s almost automatic to put patients into categories. We have our easy patients and we have our hard patients.
Someone who is young, motivated, body aware and has healthy beliefs about movement and pain can easily fall into the easy category.
But what constitutes a hard patient? There can be a number of factors, but for the most part, I’ve found it can include a combination of all four of these factors:
-
Inactive
-
Unmotivated
-
Unrealistic expectations
-
Less than adaptable body structure (poor posture, poor muscle tone, etc)
This patient archetype can be a real challenge for even the most experienced of clinicians.
I was just talking to a physio friend last week about this type of patient and how draining and hopeless she can feel after seeing these patients. In her situation, they come in with neck pain and are looking for a magic cure. They tolerate very little hands-on treatment and can flinch at the first sign of body contact.
It can be really disheartening to have this patient archetype on your caseload. It’s easy to feel like the situation is hopeless and as therapists we can easily resign ourselves to going through the motions with doing half-hearted treatments.
In this blog post, I want to help you get unstuck with this patient archetype and help you reframe your approach to treatment. My goal is to move you from a place of disillusionment and despair to a place of flow where you can be curious, collaborative, and creative. While these patient archetypes will still likely be challenging, my goal is to give you a fresh perspective to help you avoid the drain, frustration and exhaustion.
Before we dive into going through treatment strategies, I think it’s important to look at some common pitfalls that impact our ability to engage fully with our patients. Before we talk about how to approach different treatment ideas, it’s important to review our headspace. Shifting our thinking will matter more than any specific treatment, exercise or modality used with the patient.
There are four pitfalls that I believe we make with these patients:
Pitfall #1: We put everything on our shoulders
It is very easy to believe that it’s 100% up to us to get our patients better. With this patient archetype, I’ve found they can often assume that the onus is all on the therapist to get them better- that’s why they’ve come to see you. Feeling like everything is up to us can really stifle creativity, communication and collaboration with this type of patient.
Pitfall #2: We try to manufacture motivation for them
As physiotherapists, when we come across an unmotivated patient, all too often our first instinct is to try and manufacture motivation for them. We might think that we can muster up enough motivation to build momentum for them in their recovery. But as I’m sure you’re aware, this is impossible to sustain and often times our own efforts to instill motivation in our patient can actually create resistance in our patients.
Pitfall #3: We chase symptoms
As a physiotherapist, it can be tempting to focus exclusively on treating symptoms. And the further we slide into a place of frustration with this patient archetype we can easily stop being curious. We then stop exploring the other potential drivers of their pain and dysfunction.
Pitfall #4: We ignore patient resistance
One of the biggest pitfalls we can make when engaging with this patient archetype is ignoring their resistance.
-
We pretend that they’re motivated.
-
We pretend that they’re on board with doing exercise.
But reality paints a different story.
They exhibit limited motivation. They aren’t doing any of the exercises you’ve prescribed. They talk about how they find manual treatment helpful, but wince when you touch them.
So what can we do about this? I’m going to paint a path forward so we can begin to approach treatment with increased clarity and structure. I have organized treatments into three themes or buckets that will help you get results no matter what patient archetype you are dealing with.
A Path Forward to Get Results
It’s easy to get flustered when one treatment approach doesn’t work and then we jump to another treatment approach. That can quickly result in feeling disoriented and unsure of how to approach treatment.
By organizing treatment into themes or buckets, you can organize your treatment approach and the emphasis based on the treatment bucket.
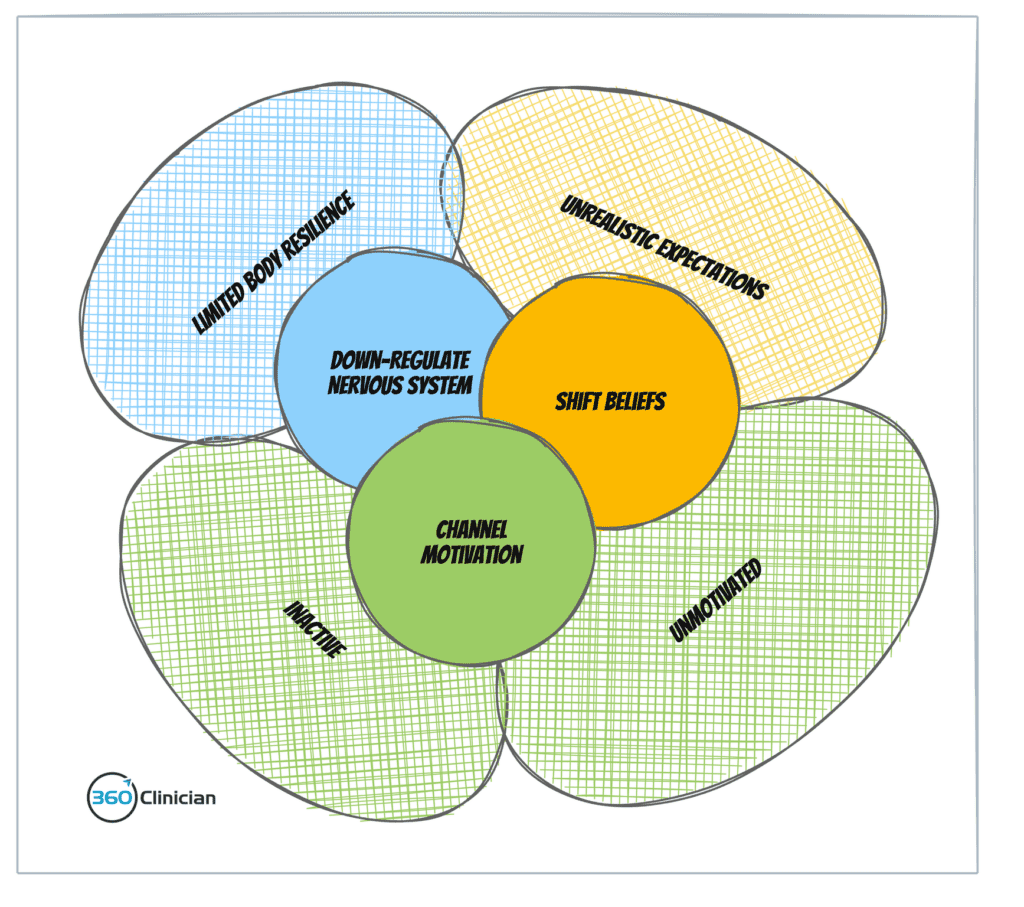
I have found that there are three treatment buckets that are necessary to get results with this patient archetype and one that doesn’t rely on poorly tolerated manual therapy.
Treatment Bucket #1: Downregulate the nervous system
When patients are sensitive to any kind of manual therapy, it’s important to have different strategies to downregulate the nervous system.
Breathing Intervention: Breath is an important nervous system regulator. And it’s something that you can use on different levels. In pain science training I did with Neil Pearson, he highlighted experimenting with both breath awareness and breath regulation. From his experience patients respond differently to different breathing strategies.
Breath Awareness: Have the patient focus on being aware of their breath – both inhale and exhale. They are not trying to control their breath. They are just aware of it.
Breath Regulation: Have the patient control the length of inhale and exhale. For example, they breathe in for 3 counts and out for 4 counts. Find a comfortable rhythm and one they can sustain for 1-2 minutes.
In testing what’s most beneficial for the patient I’ll run an experiment where they engage in an assisted movement (e.g. shoulder flexion) while doing the breathing technique. Once one version of breathing with movement is completed, I then retest an aggravating movement. If there is no change, we then run the experiment with the other breathing technique.
During these experiments, I provide simple explanations of the power of breathing to influence the nervous system, improve oxygenation and how sensitive nerves are to oxygen levels.
Free the Diaphragm: Another way that I use breathing is that I focus on addressing breathing pattern dysfunction. Oftentimes, this patient archetype has a poorly functioning diaphragm. They may be apical breathing or may have limited diaphragm contraction ability. I’ve found it beneficial to perform manual therapy and breathing instruction to assist in improving diaphragm and rib mobility.
Harness Sleep: It is important to understand if this patient archetype has disrupted sleep. Sleep is an important modulator of the nervous system and helps to downregulate the nervous system. I’ve found that patients who are struggling with persistent pain can often experience breakthroughs by addressing sleep.
Treatment Bucket #2: Shift patient beliefs
With this patient archetype, they have some pretty entrenched views about their pain and body. They can believe that it’s up to someone else to fix them, that there is a magic cure and that treatment is something that is done to them.
Trying to treat within this patient paradigm is near impossible and one that is likely destined for treatment failure.
It’s important to begin to shift and challenge the patient’s beliefs toward their body. They need to understand that there is no magic cure and treatment requires both patient and therapist working together.
This sounds easy, but I’ve found that how you approach these conversations is paramount.
Beliefs are shaped by one’s perception of reality. It’s important to challenge one’s perception of reality in order to begin shifting beliefs. If this patient archetype believes they need hands-on therapy, but can’t tolerate light touch, we have a problem. I’ve found it helpful to highlight the discrepancy to the patient.
I might say to the patient: “I know we agreed that we’d incorporate some hands-on therapy to help your neck, but I’m seeing that your body is quite sensitive whenever I start to work on your neck. Wouldn’t you agree? I think it’s important that we look at some other options that may be better tolerated by your body.”
Rather than putting the onus on yourself to come up with all the solutions (See Pitfall #1) it’s important to begin to shift to a collaborative approach. I provide some other options and come to a joint decision with the patient.
Treatment Bucket #3: Channel patient motivation
It’s easy to fall into the trap of assuming you as a physiotherapist are responsible for motivation, especially when we want our patients to succeed and get better. But it’s not up to us to create motivation for our patients.
Instead, we must step into our role as a health coach and help them find a source of sustainable motivation to support them moving forward.
For this patient archetype who has few if any movement habits, I focus initially on building a simple movement habit. I focus on consistent action that is easy for the patient to do and does not wind up the nervous system. For example, for this patient archetype with neck pain, I may have them start with some shoulder slides up the wall. They feel comfortable doing the exercise and they see the connection between the shoulders and neck (it’s meaningful).
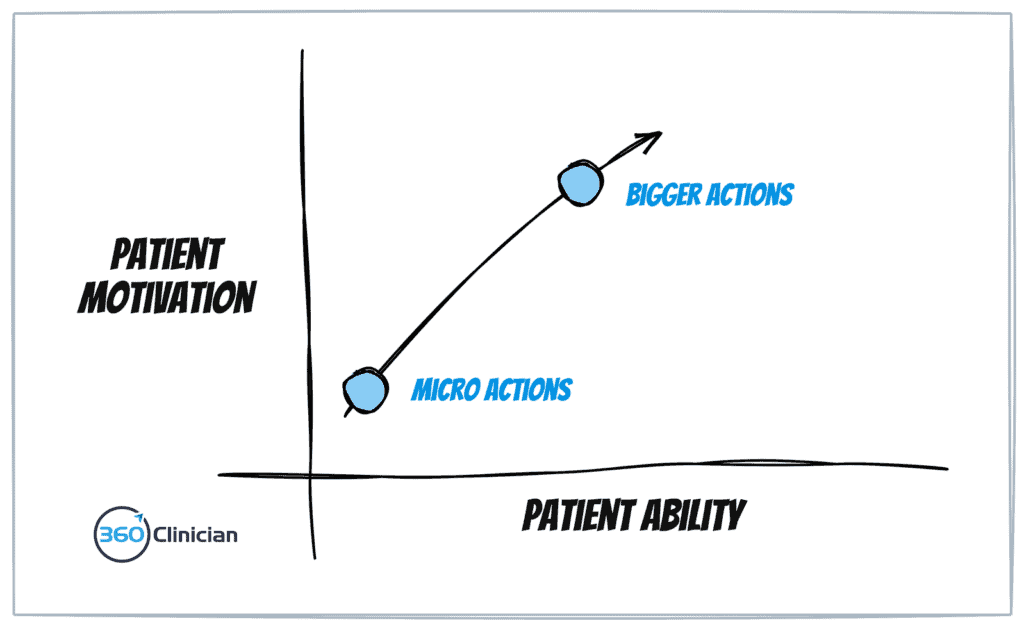
Then I write down the micro action on an index card along with the frequency to be done each day (I cover a system that I’ve developed in my exercise adherence workshop). I then proceed to make an agreement with the patient. I ask about their confidence in doing this on a daily basis and then adjust the action parameters so that their confidence is high.
Something that helps overcome hesitancy on the part of the patient is to frame this micro action within the context of an experiment. We’re doing a time-limited experiment and then taking stock after X number of days to re-evaluate if it’s something that should continue.
Once a patient is consistently performing a micro-action, I then look to move to a more challenging and likely more specific exercise (or I may add to the existing action). Getting the patient to be successful in regularly completing a simple micro action is an empowering step in the patient’s recovery journey. You’ve shifted the relationship from one where the patient expects all the answers from you the therapist, to one where there is a collaborative partnership where the patient is building self-efficacy and autonomy.
Wrap Up
This patient archetype may be challenging to treat, but when you identify and troubleshoot the pitfalls, you can move forward by reframing treatment within one of the three buckets I walked through.
To better flow,
Andrew
If you enjoyed this article and want to stay up-to-date on my newest content, sign up for the Clinical Flow Newsletter! There you will have access to special offers, exclusive content, and be part of a growing community of clinicians with the purpose of improving yourself and your clinical practice.

