Anxiety.
It can range from minor annoyance to crippling.
And there’s no lack of opportunities to feel anxiety when seeing patients. Whether it’s an assessment that is running behind, a more complex assessment than expected, or a patient who appears to be rapidly losing motivation for treatment.
I’m no stranger to anxiety and have found it to be an important emotion to navigate to help move into a place of consistent clinical flow.
In my last blog, I talked about Clinical Flow and the important role it plays in both work engagement, burnout prevention and clinical performance. Mihaly Csikszentmihalyi is the foremost expert on the flow state.
He created a zone of flow – a sweet spot between skill and challenge. When our skill level matches the challenge of the activity, we are in a better place to enter into a state of flow. When the challenge is high and skill is low, the outcome is anxiety and we are far removed from flow.
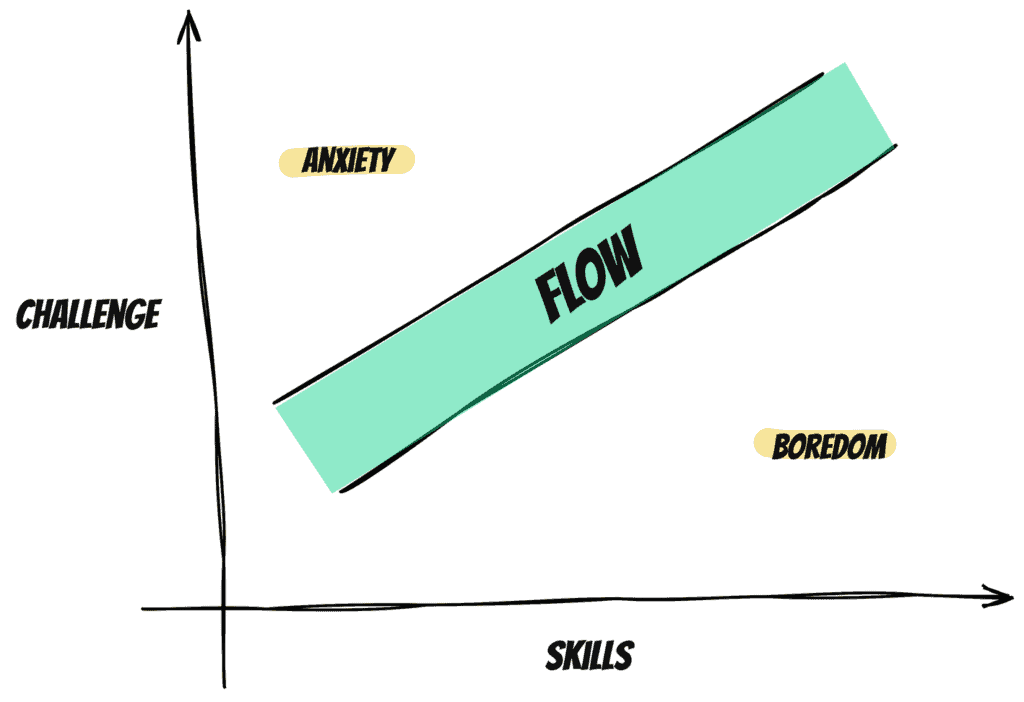
When looking through this lens, it makes sense that one way to support working in flow is to improve our skill level. And skill improvement is a valid and important aspect to support operating in a flow state. The reality however is that our skills are constantly challenged by ever-changing complex situations.
Another way to reduce anxiety would be to reduce the level of challenge. However, within physiotherapy practice, it’s not all that easy to dictate the patients that see us or the level of challenge that they present to us.
I believe that we can manage how we interact with the challenges we experience in clinical practice. By modulating our perception of the challenges we encounter we can respond in a way that doesn’t result in increased anxiety.
Here are 6 strategies that I use to help reduce my anxiety level:
#1 Treat what you see
This was recommended during one of my clinical placements and it’s something that has stuck with me. It’s a mantra that I remind myself of regularly when I find my anxiety levels rising. When we’re dealing with a challenging assessment, we can feel pressure to try to get to the root cause. But the reality is that sometimes there’s so much going on that it’s hard to know what’s causing a problem versus what is the result of the problem.
We can put undue pressure on ourselves to figure it all out, and all in one session no less! I’ve found this to be a very effective release valve as it takes away some of the internal pressure that increases anxiety.
#2 Focus on the basics
This has been another valuable reminder that I use when my anxiety levels start to elevate. But what do “the basics” mean?
It includes:
- Taking a detailed patient history
- Screening for red flags
- Completing a neuro exam
- Evaluating range of motion and strength
- Basic palpation of affected areas
As I’ve written about in other blog posts, stress decreases our perceptual awareness and ability to process effectively. When we focus on the basics, it helps us get out of our heads by taking concrete action.
I’ve often found that when I’m doing “the basics” I can still feel anxious because I don’t know the outcome of the assessment. In those situations, I remind myself to trust the process and be ok with not knowing for a few moments in time.
#3 Principle-based treatment
Another important strategy is focusing on principle-informed action to help to navigate the complexities we face every day with patients. When anxiety begins to build and things are getting muddied in my mind, I find it is helpful to step back and ask myself the relevant principles at play.
There are many different principles you can lean on, but here are a few examples:
- Tissue healing times
- Tendon loading principles
- Level of tissue irritability
- Active listening principles
#4 Challenge the self-talk
Anxiety is often exacerbated by our own perfectionist tendencies. We put pressure on ourselves which can make it difficult to navigate complex clinical situations. It can be helpful to listen to your self-talk and listen for key words that highlight unhealthy thinking such as:
- “I must”
- “I should”
- “I need”
I’ve found it helpful to reframe how I speak to myself. Rather than saying “I must figure this out in this assessment”, I could reframe it to “It would be great to figure this out in this assessment, but it’s ok if I don’t. I’ll be ok either way.”
#5 Be okay with changing your opinion
I’ve found in my own practice that a lot of anxiety can come from the pressure I put on myself to figure everything out right away. When I shifted to approaching my assessments with a hypothesis-driven approach, I found the pressure dissipated. It allowed me to have a diagnostic impression, that would be validated in subsequent sessions. If things changed, I was ok with it because new information often came to light including treatment response (or lack of response) from the patient.
#6 Look at the whole person
I’ve found that my anxiety can increase when I hit a roadblock with treatment. Maybe the patient isn’t progressing as expected or the treatment response I was expecting doesn’t materialize. In those situations, I find it helpful to zoom out and look at other factors that could be at play.
What other psychosocial areas have I potentially missed?
What could be hindering progress?
Looking at aspects such as sleep health, pain beliefs, social supports, etc. can all be valuable areas to explore.